Lorente-Pascua J1, Lao-Domínguez FA2, Fobelo-Lozano MJ2, García-Bernal AM1
1 Área de Gestión Clínica Sur de Sevilla. Hospital Virgen de Valme Ophthalmology Departament. Seville (Spain)
2 Área de Gestión Clínica Sur de Sevilla. Hospital Virgen de Valme. Pharmacy Department. Seville (Spain)
Fecha de recepción: 06/03/2022 – Fecha de aceptación: 01/04/2022
Correspondencia: José Lorente Pascua – Hospital Virgen de Valme – Ctra. de Cádiz Km. 548,9 – 41014 Sevilla (España)
jlorentepascua@development
____
Summary
Objetive: To report the clinical course of a case series of patients with persistent epithelial corneal defects (PECD) treated with insulin eye drops.
Method: Retrospective review of five patients -four non-diabetic and one diabetic- in treatment with insulin eye drops 1 U/mL four times a day (QID).
Results: Patients developed refractory epithelial ulcers due to different etiology (three infections, one trauma and one chemical injury). After treatment with topical insulin all defects were healed in about 30-60 days.
Conclusion: Insulin formulated as 1 U/mL eye drops and administered QID can be an effective and safe option for PECD.
Key words: Topical insulin, persistent epithelial corneal defect, corneal wound healing, case report.
Colirio de insulina para defectos corneales epiteliales persistentes. Una serie de casos
Resumen
Objetivo: Comunicar la evolución clínica de una serie de casos de pacientes con defectos corneales epiteliales persistentes (PECD) tratados con colirio de insulina.
Método: Revisión retrospectiva de cinco pacientes –cuatro no diabéticos y uno diabético– en tratamiento con colirio de insulina 1 U/mL cuatro veces al día (QID).
Resultados: Los pacientes desarrollaron úlceras epiteliales refractarias de diferente etiología (tres infecciones, un traumatismo y una lesión química). Tras el tratamiento con insulina tópica todos las lesiones se curaron en unos 30-60 días.
Conclusión: La insulina formulada en forma de colirio de 1 U/mL y administrada QID puede ser una opción eficaz y segura para la PECD.
Palabras clave: Insulina tópica, defecto corneal epitelial persistente, cicatrización de la córnea, caso clínico.
____
Introduction
Epithelial corneal defects are damaged areas of the corneal epithelium as a consequence of an injury caused by a trauma, infections, neurotropic disease or even corneal dryness. When an injury occurs, the cornea typically regenerates in a few days. However, some cases may require of more time to heal. In those cases in which a corneal lesion does not heal after two weeks, it is considered as a persistent epithelial corneal defect (PECD).
Current management of PECD is challenging. Standard of care includes ocular lubricants, ointment and patching which frequently fails, requiring more complex therapies such as surgical interventions. Novel treatments for PECD which have a mechanism focused on the regeneration of nerve cells or the extracellular matrix architecture have been proposed1. Among all of them, insulin has been proposed as a promising treatment for PECD1,2. However, clinical experience with insulin eye drops is limited and more evidence in both diabetic and non-diabetic patients is still needed. Here we present a five case series of PECD patients treated with insulin eye drops at 1 U/mL.
Cases description
Five cases of patients being treated with insulin eyedrops (1 U/mL) are described, one of them with diabetes mellitus type I and the other non-diabetic. Administration frequency was 4 times in a day (QID) similar to Wang et al.3 All patients continued with treatment after epithelial healing.
Case 1
A 47 year-old man, non-diabetic, with a penetrating keratoplasty due to ocular caustication three years ago. He presented a persistent epithelial defect during one year despite treatment with amniotic membrane, autologous serum and hyaluronic acid tears. We have previously reported this case in which the patient started treatment with topical insulin at a dose of 50 U/mL achieving PECD healing in two months4. However, it was decided to keep maintenance treatment with a reduced dose of insulin at 1 U/mL QID to avoid corneal defect recurrence. A year after, he continued asymptomatic with insulin eyedrops.
Case 2
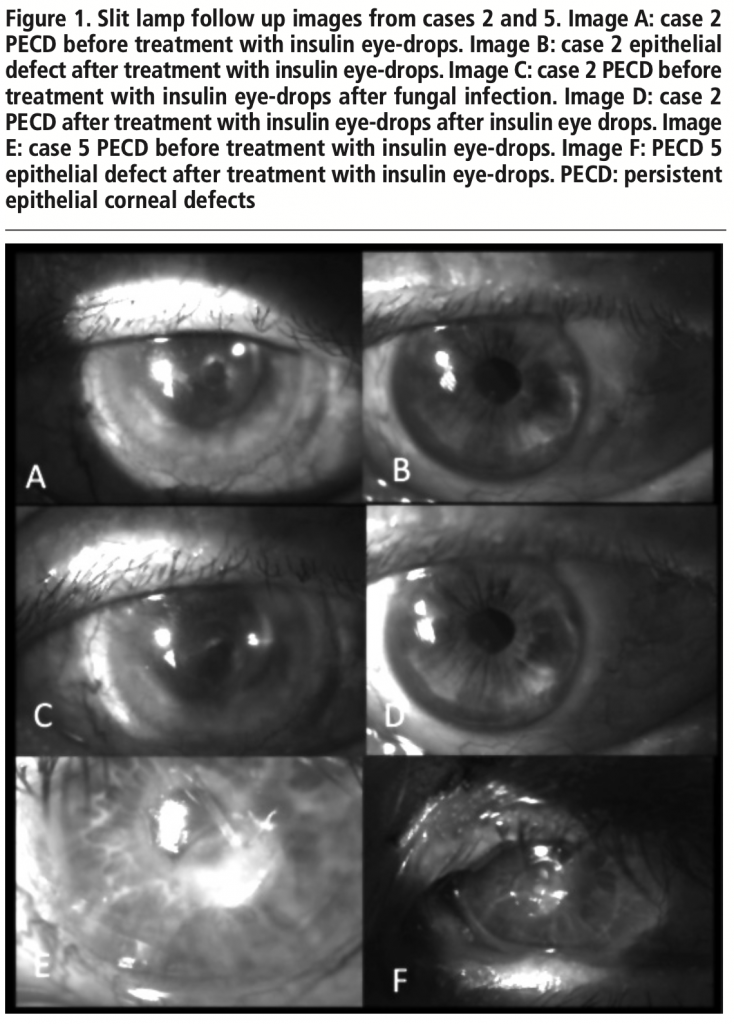
A 79 years-old woman, non-diabetic, with PECD due to herpes keratitis (figure 1A) since two months treated with bandage contact lens and hyaluronic acid tears. She started using insulin eye drops then and two months later her corneal epithelium healed (figure 1B). Three months after that, she had to stop treatment because the patient suffered a fungal infection; when infection was controlled (figure 1C), insulin eye drops were restarted and PECD healed again (figure 1D).
Case 3
A 76 years-old woman, non-diabetic. She was treated with penetrating keratoplasty due to herpes keratitis. Two years later, an epithelial defect persisted during two months more despite management with bandage contact lens and hyaluronic acid tears. Insulin eye drops were then prescribed with epithelial and stromal healing in about 1 month.
Case 4
A 35 years-old woman, non-diabetic, with penetrating keratoplasty due to trauma twenty years ago. She presented an epithelial defect with stromal thinning. After two months of failure of hyaluronic acid tears treatment, insulin eye drops were initiated. One month later, stromal thinning was fully resolved.
Case 5
A 72 years-old woman, diabetic, with a history of neurotrophic keratopathy due to facial palsy, which required of lateral tarsorrhaphy. However, she suffered bacterial keratitis with a 3 mm defect treated with topical voriconazole, ceftazidime and vancomycin (figure 1E). After oral doxycycline and hyaluronic acid tears for the time of one month the lesion persisted, so she was treated with insulin eye drops with epithelial healing in one month (figure 1F).
Discussion
It is unknown how instilled insulin in the eye promotes corneal healing. Under normal conditions, insulin stimulates normal endothelial function, but in the presence of insulin resistance its action on the endothelium leads to the development of endothelial dysfunction5. The existence of insulin and insulin-like growth factor receptors in cornea keratocytes and epithelial cells has been described, which could explain the increment on the corneal epithelial healing rates6.
In our serie, we presented five cases of one diabetic and four non-diabetic patients with PECD from different etiology refractory to conventional treatment. All patients presented epithelial healing in about 30-60 days similar to others reports described in the literature. Wang et al. reported a six patients series treated with 1 U/mL QID topical insulin in which only one was indicated to be diabetic3. All cases succeed with re-epithelization within seven up to twenty-five days. A larger PECD series with insulin eye drops 1 U/mL QID reported an epithelial healing of 81% after a month of follow-up and complete re-epithelization after a meantime of thirty four days7. Both series presented an heterogeneous etiology and were treated with similar dose and posology than our cases.
Recently, a case of use of topical insulin in a neurotrophic keratitis in a diabetic patient has been reported8. Patient presented bilateral chronic ulcers and no improvement with conventional treatments. 25 U/mL topical insulin was used with epithelial healing in twenty-five days. Delayed epithelial healing in diabetic patients has been reported years ago and it is believed to be due to polyneuropathy.
We also present a case where it was necessary to stop treatment temporarily due to a fungal superinfection. Besides, we observed epithelization when we restarted treatment. Also, we included among the case serie the follow-up of a patient which previously was reported to recover from PECD thanks to topical insulin at 50 UI/mL4. Although the initial recovery was achieved with a higher dose of insulin, we consider relevant to highlight the lowering of the dose to 1 IU/mL as maintenance treatment, without showing any negative sign in her injury recovery.
Insulin eye drops have been revealed as a secure treatment3,9. However, only two patients have been using it for long-term – one of them suffering a fungal infection during the therapy period. It remains unclear if this infection can be attributed to the treatment. Nevertheless, in this case corneal epithelium was heavily damaged, so it is highly probably that fungal infection was more related to cornea state rather than insulin treatment.
In conclusion, insulin formulated as 1 U/mL eye drops and administered QID can be a quick, effective, safe and affordable option for PECD.
Conflict of interests: The authors declare that they do not present a conflict of interest.
BIBLIOGRAPHY
1. Bremond-Gignac D, Daruich A, Robert MP, Chiambaretta F. Recent innovations with drugs in clinical trials for neurotrophic keratitis and refractory corneal ulcers. Expert Opin Investig Drugs. 2019;28(11):1013-20.
2. Zagon IS, Klocek MS, Sassani JW, McLaughlin PJ. Use of topical insulin to normalize corneal epithelial healing in diabetes mellitus. Arch Ophthalmol. 2007;125(8):1082-8.
3. Wang AL, Weinlander E, Metcalf BM, Barney NP, Gamm DM, Nehls SM, Struck MC. Use of Topical Insulin to Treat Refractory Neurotrophic Corneal Ulcers. Cornea. 2017;36(11):1426-28.
4. Serrano-Giménez R, Contreras-Macías E, García-Bernal A, Fobelo-Lozano MJ. Insulin eye drops for treating corneal ulcer in a non-diabetic patient: regarding a case. Farm Hosp. 2020;44(6):297-9.
5. Vincent MA, Montagnani M, Quon MJ. Molecular and physiologic actions of insulin related to production of nitric oxide in vascular endothelium. Curr Diab Rep. 2003;3(4):279-88.
6. Stuard WL, Titone R, Robertson DM. The IGF/Insulin-IGFBP Axis in Corneal Development, Wound Healing, and Disease. Front Endocrinol (Lausanne). 2020;11:24.
7. Diaz-Valle D, Burgos-Blasco B, Gegundez-Fernandez JA, Garcia-Caride S, Puebla-Garcia V, Peña-Urbina P, Benitez-Del-Castillo JM. Topical insulin for refractory persistent corneal epithelial defects. Eur J Ophthalmol. 2020: 1120672120958307.
8. Tong CM, Iovieno A, Yeung SN. Topical insulin for neurotrophic corneal ulcers. Can J Ophthalmol. 2020;55(5):e170-2.
9. Fai S, Ahem A, Mustapha M, Mohd Noh UK, Bastion MC. Randomized Controlled Trial of Topical Insulin for Healing Corneal Epithelial Defects Induced During Vitreoretinal Surgery in Diabetics. Asia Pac J Ophthalmol (Phila). 2017;6(5):418-4.
____
