Plo-Seco I, Sáez López P, Roldán Navarro P, Sáez Nieto C, Sanz Márquez S, Pérez Encinas M.
Hospital Universitario Fundación Alcorcón (Madrid, ES)
Fecha de recepción: 20/02/2023 – Fecha de aceptación: 21/03/2023
Correspondencia: Isabel Plo Seco · Hospital Universitario Fundación Alcorcón. Servicio de Farmacia. Calle Budapest, 1, 28922 Alcorcón, Madrid · iploseco@gmail.com
____
Abstract: Potentially inappropriate prescriptions (PPIs) are very common among the elderly population.
Background: Potentially inappropriate prescriptions (PIP) are very prevalent among the elderly population. This leads to a major ratio of adverse reactions to medication.
Aims: To know the prevalence of PIP in elderly patients, classify them and make interventions to reduce the amount of PIP in patient’s prescriptions
Methods : Ambispective multidisciplinary interventionist study (February- 2019 – February 2020) on patients over or equal 70 admitted to the Trauma Unit of a general university hospital. Patients with admissions of less than 48 hours or in a terminal state were excluded. All patients underwent a comprehensive geriatric assessment and complete revisions of their home and admission treatments. PIP were identified by applying a checklist tool based mostly on START/STOPP, Less Chron and Beers criteria. After identifying PIP, we classified them and carried out different kinds of interventions. Six months after, we verified that they had been successful.
Results: 286 PIP were identified in 199 patients. The most prevalent interventions were deprescription (36.0%), dose adjustment (32.2%) and omission of a prescription (18.9%). Six months after we reviewed the home treatments of patients with interventions. The mean number of PIP in this group of patients decreased from 1.71 (SD:1.1) to 0.75 (SD:0.93), (p<0.001) and polypharmacy was reduced from 9.83 (SD:4.40) drugs per patient to 9.23 (SD:4.55), (p<0.05).
Conclusion: The collaboration between hospital pharmacist and geriatrician allows the detection of PIP and the proposal of personalized alternatives adapted to the individual conditions of each patient that lead to an enduring improvement in the quality and safety of the prescriptions.
Keywords: geriatrics, treatments, inappropriate prescription, elderly, adverse effects.
Optimización del tratamiento de los pacientes ortogeriátricos a través de un programa consensuado de revisión de recetas entre la farmacia de hospital y los servicios de geriatría
Objetivos: Conocer la prevalencia de las PPI en los pacientes geriátricos ingresados en el servicio de traumatología, clasificarlas y realizar intervenciones para minimizar sus efectos.
Método: Estudio intervencionista multidisciplinar ambispectivo (febrero-2019-febrero2020) en pacientes de 70 años o mayores, ingresados en la Unidad de Traumatología de un hospital general universitario. Se excluyeron los pacientes con ingresos inferiores a 48 horas o en estado terminal. A todos los pacientes se les realizó una valoración geriátrica integral y revisiones completas de sus tratamientos domiciliarios y hospitalarios. Las PPI se identificaron aplicando una lista de comprobación consensuada basada principalmente en los criterios START/STOPP, Less Chron y Beers. Tras identificar las PPI, las clasificamos y llevamos a cabo distintos tipos de intervenciones. Seis meses después, comprobamos si nuestra intervención permanece.
Resultados: Se identificaron 286 PPI en 199 pacientes. Las intervenciones más prevalentes fueron la deprescripción (36,0%) y el ajuste de dosis (32,2%). Seis meses después se revisaron los tratamientos domiciliarios de los pacientes con intervenciones al alta. El número medio de PPI por paciente pacientes disminuyó de 1,71 (DE:1,1) a 0,75 (DE:0,93), (p<0,001). La polifarmacia se redujo de 9,83 (DE:4,40) fármacos por paciente a 9,23 (DE:4,55), (p<0,05) después de nuestra actuación.
Conclusión: La colaboración entre farmacéutico de hospital y geriatra permite la detección de PPI y la propuesta de alternativas personalizadas adaptadas a las condiciones individuales de cada paciente que conducen a una mejora duradera en la calidad y seguridad de las prescripciones.
Palabras clave: geriátrico, deprescripción, polifarmacia, seguridad, traumatología, efecto adverso.
____
Introduction
Secular trends of population aging and disease chronification have facilitated a new profile of patient characterized by presenting pluripathology, which is inherently associated with the prescription of complex polytherapy. Polymedication entails a high risk of interactions and adverse reactions to drugs, as well as medication errors, therapeutic cascade and low adherence to treatment1, 2
A potentially inappropriate prescription (PIP) is one whose risk of producing adverse effects is greater than the expected clinical benefit of its use, especially when there is evidence of the existence of safer and/or more effective therapeutic alternatives. It also includes the omission of clinically indicated drugs, the use of drugs with a different frequency or duration than indicated and the presence of therapeutic interactions and duplicities.
Several studies showed a high prevalence of PIP among older adults which leads to a major ratio of adverse reactions to medication. All of these events result in an unnecessary increase in health care demand, taking into account that 5-20% of hospital admissions of older patients are caused by adverse events associated with medication, many of which preventable3, 4. The application of different strategies for optimizing treatments in elderly patients has shown a reduction of polypharmacy, and consequently, of fragility, according to the literature5, 6. Interventions must be adapted to the settings and patients’ needs and the best results in improving important health outcomes, such as readmissions or emergency room visits, have been shown in multifaceted multidisciplinary interventions7.
On the other hand, it is important to remind that there is limited knowledge of the efficacy and safety of treatments in elderly patients, given that they are usually excluded from clinical trials8. In addition, clinical practice guidelines are focused on isolated pathologies and rarely include specific therapeutic recommendations for pluripathological patients, as most elderly patients are9. In this context, a systematic review of patient’s individual needs and a comprehensive geriatric assessment is necessary, adapting the treatment to the evolution of the functional and cognitive situation.
Several studies have demonstrated the importance of the role of the hospital pharmacist collaborating with the physician responsible for the patient in the review of treatment during admission and discharge from hospital10 so that it is important their inclusion in the multidisciplinary team to promote a rational use of medication.
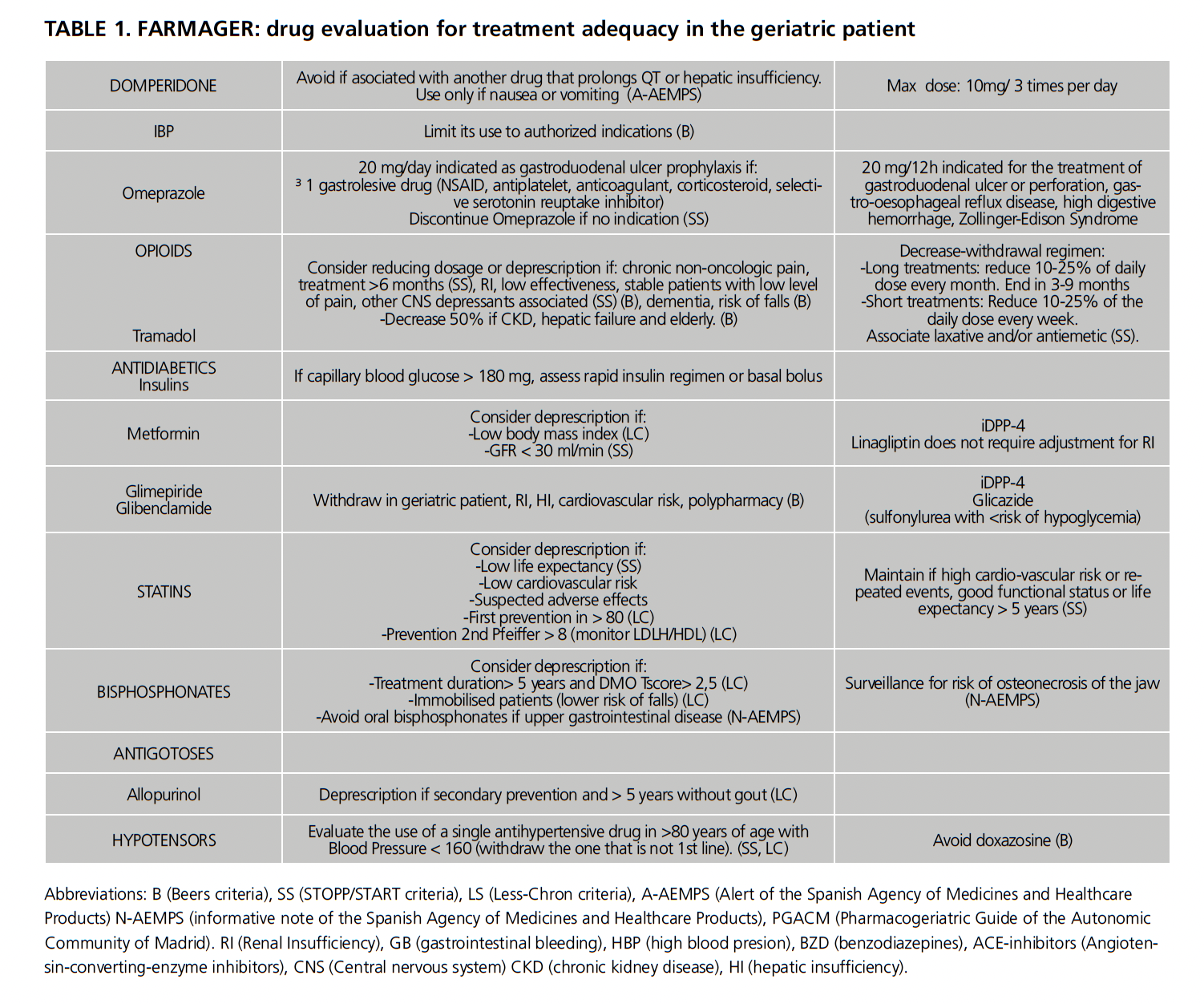
Due to the above, we started a pilot project of intervention in elderly patients admitted to the Traumatology Unit of the hospital for more than 48 hours, beginning a collaboration between pharmacy and geriatrics service. In order to facilitate the detection of PIP in old patients’ prescriptions we designed a working tool that we called FARMAGER. In the present study, we aimed to measure the prevalence of PIP among old patients, classify them and make interventions to improve the quality and safety of their admission and home treatments.
Methods
We carried out an ambispective multidisciplinary interventionist study (February 2019-February 2020) on patients over or equal 70 years old admitted to the Traumatology Unit of the University Hospital Foundation of Alcorcón. Patients younger than 70, with hospital admissions of less than 48 hours or in a terminal state were excluded. The study was performed in three phases.
Phase one
During the first two months, we created a work tool called FARMAGER with the objective of facilitating the systematized review of treatments and the detection of PIP. For its design, we selected some drugs and pharmacological groups in order to prioritize our intervention in them, proposing doses and therapeutic alternatives suitable for the elderly patients. We based the selections of these drugs and the recommendations given in different international explicit methods of identification and adequacy of PIP based on evidence and expert consensus as: the Beers criteria 201911, the Screening Tool of Older Person’s Prescriptions/Screening Tool to Alert doctors to Right Treatment (STOPP/START criteria)12 and the List of Evidence-Based Deprescribing for Chronic Patients (Less-Chron criteria)13.
We also used the Pharmacogeriatric Guide of the Autonomic Community of Madrid (PGACM)14 and the alerts and information notes of the Spanish Agency of Medicines and Healthcare Products (AEMPS) that could specially affect older patients15, 16, 17, 18, 19, 20, 21.
Furthermore, during this phase, we updated a specific template in the electronic admission medical record adapted to the orthogeriatric patient that contains analgesics, heparin, laxatives and psychotropic drugs, with its adjusted doses and posology.
Finally, we prepared information sheets to inform patients upon discharge about the indications, correct use and risk involved with benzodiazepines to complement the oral information given by the doctor at this point.
Phase two
In the second phase (April-June 2019) we implemented a structured review of the treatments.
During the first 24-48 hours after the admission, a geriatrician performed a detailed comprehensive geriatric assessment including cognitive function, frailty and functional dependence. After the interview, the geriatrician initiates the adaptation of the pharmacological treatment. Meanwhile, a pharmacist validated the pharmacological treatment using the patient’s electronic medical records, analytical parameters and both electronic home prescription and electronic hospitalization prescription. The pharmacist verified that chronic treatment was well scheduled and adjusted to the patient’s acute situation. We also verified that there were no pharmacological duplicities or interactions, that prescriptions were optimal in the elderly patient and that doses were correctly adjusted to the current renal and hepatic function. To detect PIP and propose alternatives we applied FARMAGER.
At the end of the morning, a brief meeting between pharmacist and geriatrician was conduced where we discussed the possible interventions. The intervention strategies were different depending on where we found the PIP and the type of PIP detected. The possibilities were the following:
If the intervention was made on electronic admission prescription:
Direct modification of the prescription
Recommendation to the traumatologist in charge.
If the intervention was made on electronic home prescription:
Direct modification of the prescription.
Communication with the primary care doctor in charge.
Recommendations in the discharge report.
If possible, modifications in chronic treatment were carried out gradually and started during the admission to control any possible adverse effect. When patients leaved the hospital, any change in their treatments was explained and discussed with them.
For the evaluation of the program, we collected the following variables: age, sex, diagnosis on admission, comorbidities, number of drugs as usual home treatment, number of drugs during admission (the day the first evaluation was performed), number of PIP in home treatment, number of PIP during admission, number of interventions performed, type of intervention and therapeutic group concerned.
The interventions were coded as: deprescription, dose adjustment, detection of therapeutic duplicity, adjustment of treatment duration, adjustment of treatment frequency, omission of a prescription and change of administration route. It was specified whether the intervention was carried out on chronic treatment or on hospital prescription. Polifarmacy was defined as number of chronic drugs prescribed equal or major 5.
Phase three
In the last part of the project (February 2020) a backward review was carried out to determine the real impact of the program. Using the electronic home prescription we checked if the interventions performed on the chronic treatment had succeeded six months after. We also recorded the number of drugs prescribed at this moment.
Ethical considerations
This study was approved by the hospital Ethics Committee for Research with medicinal products. The interventions were considered by the committee to be a part of the routine clinical practice and therefore no written consent was requested.
Statistical analysis
Absolute and relative frequencies were used to describe the distribution of the qualitative variables and mean and standard deviation (SD) or median and interquartile range (IQR: p25-p75) were used to describe the distribution of the quantitative variables, depending on the distribution of the data.
For the comparison of PIP and polypharmacy six months after the intervention, first we performed a normality test (Kolmogorov-Smirnov) and after we applied Student’s t-test. All tests were considered bilateral and those p-values lower than 0.05 were considered statistically significant. For data analysis we used the statistical program Stata MP, 16.0 version.
Results
FARMAGER contains 26 drugs and 11 pharmacological groups and includes 48 recommendations; 14 of them are general recommendations for pharmacological groups and 34 are specific recommendations for specific drugs.
Of these 48 recommendations, 17 were taken from Beers criteria, 15 from STOPP/START criteria, 11 from Less-Chron criteria, 7 are alerts and notes from the AEMPS and 2 are based on the PGACM (4 of them are based in two criteria that overlap). The 11 pharmacological groups comprised are anticholinergics, anticholinesterase drugs, antihypertensive drugs, bisphosphonates, hypnotics, thiazide diuretics, non-steroidal analgesics (NSAID), opioids, proton pump inhibitors, statins and tricyclic antidepressants. We can see the full table as Table 1.

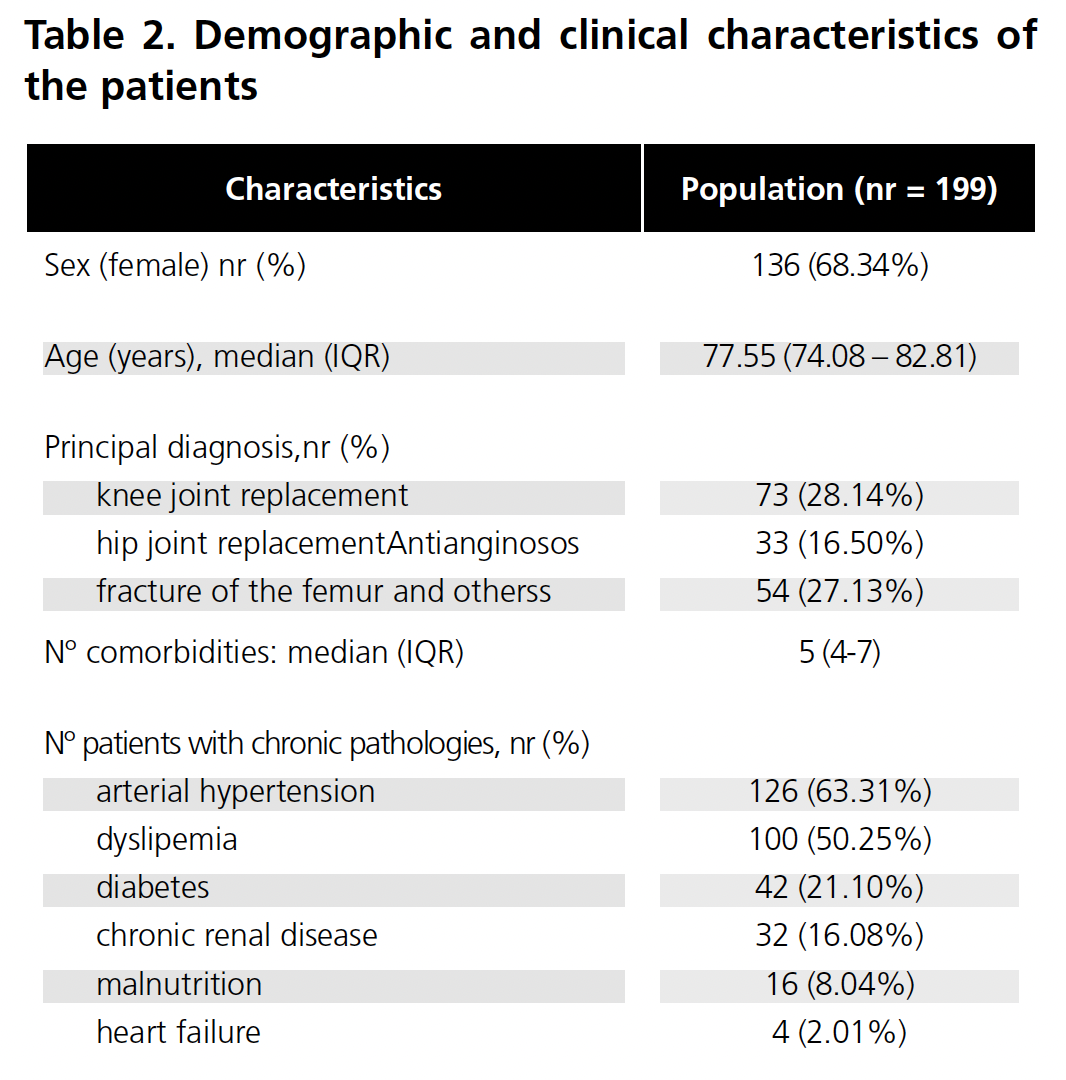
Of the total number of patients admitted to the Traumatology Unit during the study period, 199 were included, 91.2% of the total amount who met the inclusion criteria. The baseline characteristics of the patients included in the study are shown in Table 2.
Polypharmacy in chronic domiciliary treatment was detected in 73.1% of patients (CI95%: 66.5%-78.8%), with a median of 8 drugs (IQR: 5-10) per patient. During hospitalization 97.0% (CI95%: 93.6%-98.6%) of the patients took more than 5 drugs, with a median of 10 drugs (IQR: 8-12) prescribed.
We identified 286 PIP in the sum of domiciliary and hospital treatments of the 199 patients included in the study, with a median of 1 PIP (0-2) per patient. Of all patients, 46 had PIP in their home treatment, 71 had PIP in their hospital treatment, 17 had PIP in both home and hospital treatments and 65 had no PIP.
We made one intervention in 30.2% of patients, two interventions in 15.1% and three or more interventions in 13.6%.
Up to 39.9% of the adjustments were to the usual chronic treatment that patients took at home and 60.1% to the treatment prescribed during admission.
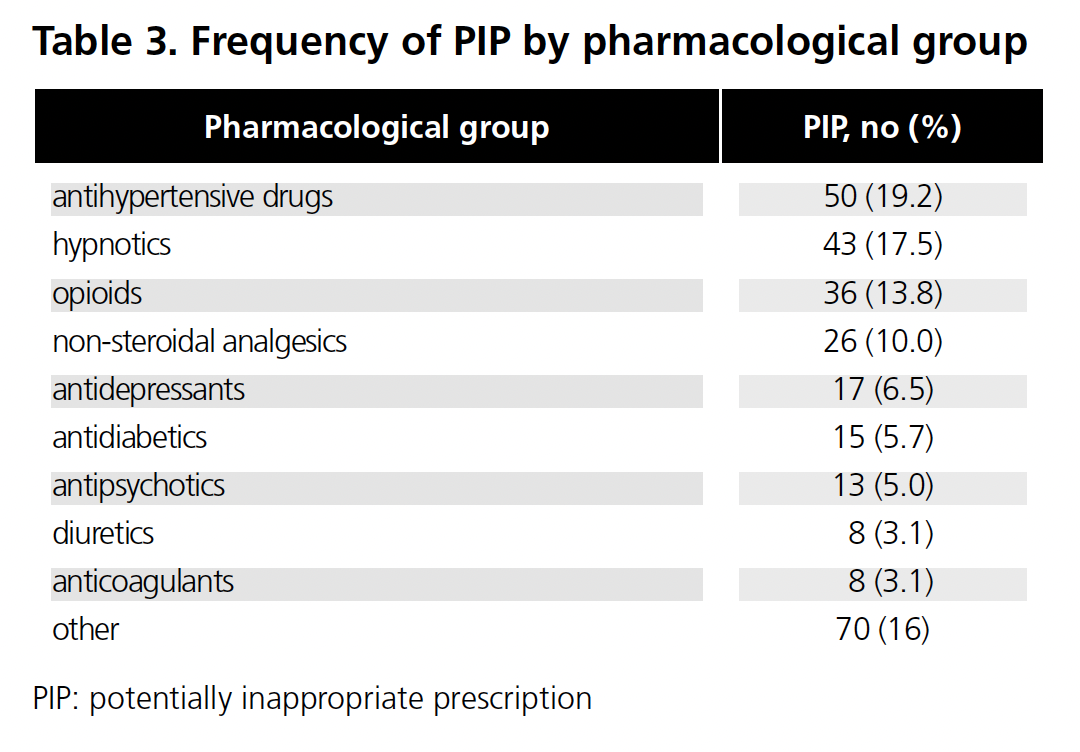
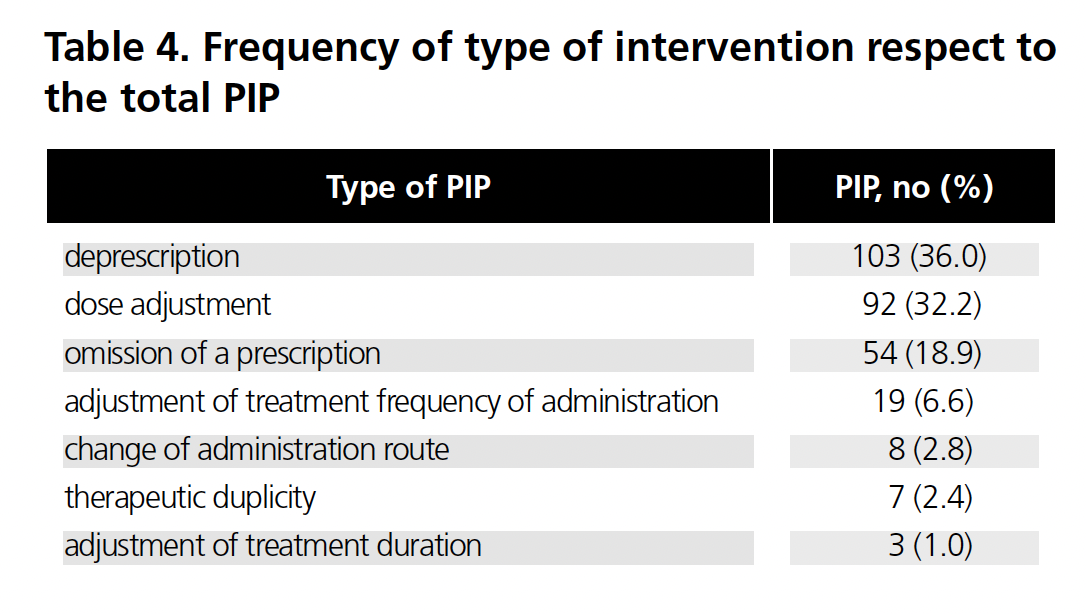
The pharmacological groups in which we detected more PIP were antihypertensive drugs (19.2%), hypnotic drugs (16.5%) and opioids (13.8%). The frequency of interventions by pharmacological group can be seen in Table 3. The majority of the interventions performed were deprescription (36.0%) followed by dose adjustment (30.8%). The type of interventions made is shown in Table 4.
The percentage of deprescription interventions on medication prescribed during admission was 23.8% and on home treatment was 54.4%. On the other hand, the frequency of dose adjustment interventions accounted for 32.6% of the hospital medication interventions while it was a 28.1% of the interventions on home treatment. New drugs were prescribed in 26.2% of the patients during admission because of our intervention (intervention coded as omission of a drug prescription), and in 7.9% at discharge.
Six months after the intervention the number of PIP on patients’ home treatment reduced significantly. Considering only the home treatments where we detected PIP, the number of PIP reduced from a mean of 1.71 (SD: 1.10) to 0.75 (SD: 0.93), (p < 0.001) and from a median of 1 (1-2) to a median of 0.5 (0-1), respectively. The Table 5 details the variation in the number of PIP between both periods classified by type of intervention.
The mean number of drugs as chronic home treatment for patients who were intervened on dropped from 9.83 (SD: 4.40) before the program to 9.23 (SD: 4.55) at six months (p < 0.05).
Discussion
The results obtained in our study indicate that more than a half of the patients equal or over 70 years old admitted to a Traumatology Unit have at least one PIP, based on the criteria of the FARMAGER program.
The percentage of patients with at least one PIP in our study was 58.9%. This result is higher than that obtained by other authors internationally, being 46% in a study in the elderly using the STOPP criteria 22 and 41% in another study applying the STOPP/START criteria 23. On the contrary, different national studies detected results similar to ours or even superior 24.
In addition, the average number of medications prescribed in our study’s patients is considered high. We have observed that polypharmacy is present in more than 70% of our patients with a median of 8 drugs prescribed for each individual. These results were higher in the case of hospitalized patients, with a prevalence of polypharmacy of 97%. We can see that PIP can occur at all points of patient care, having been detected in both home and hospital treatment. These results are in line with those of other studies carried out in similar populations 25, and are higher than the national average 26.
It should be noted that, in our study, the most frequent type of intervention at the level of chronic treatment was deprescription, and that this has being maintained for at least six months in half of the patients. In patients with polypharmacy, literature has described a general inertia to maintain the prescribed treatments27. Therefore, the high level of acceptance of deprescription in our study was noteworthy. This is probably due to the careful communication of the hospital specialists with both the primary care physician and the patient himself, who is made a part in the decision. Several studies show how deprescribing should be a shared decision with the patient and caregivers, and the importance of following up the intervention to make it last in time28.
The therapeutic groups most involved in our interventions were antihypertensives and hypnotics. These results are similar to those of a meta-analysis where benzodiazepines were positioned as the drugs most related to PIP30. A national study carried out in a social health centre where they applied the STOPP/START criteria, placed benzodiazepines and diuretics as the pharmacological groups most associated with PIP25. It is worth noting how in our study a reduction in benzodiazepine prescriptions was achieved probably thanks to the educational work focused on both health professionals and patients. The informed delivery of the information sheets that reinforced the information given by the physician at the time of discharge may also contributed to maintaining these results over time.31. NSAIDS were also highly associated to PIP in our study agreeing with bibliography says30.
In our study, 26.2% of the interventions on patients during admission were coded as omission of a drug, and therefore a new drug was proposed to be prescribed. In some cases, the omitted medication was part of the patient chronic home treatment that was not prescribed during admission by mistake, but in other cases, the collaboration between pharmacist and geriatrician allowed the detection of untreated pathologies.
FARMAGER is an easy and useful tool to detect PIP, and its implementation helps to improve the quality of the prescriptions. However, it is always necessary an individualized assessment of the prescription according to the clinic, the frailty and other circumstances of each patient. In the use of the comprehensive geriatric assessment to evaluate so, hence the necessary collaboration between pharmacist and geriatrician in this type of patient. One of the strengths of the work is therefore the multidisciplinary team, which allows to provide a global and targeted approach to the revision of the treatment of elderly patients.
On the other hand, it is as well intuited an improvement in the prescription of orthogeriatric patients during hospitalization. This may be due to our interventions during February and March 2019, which were approached from a didactic point of view. On the other hand, the implementation of prescription templates adapted to the orthogeriatric patient may have been reflected in an improvement of prescriptions. However, this trend has not been evaluated.
After completion of this study, the FARMAGER review program has being used not only in our hospital but also in the affiliated social health centers. The future would be the validation of the tool through a multicenter study and the programming of an electronic version incorporated to the clinical history as a support system for the clinical decision.
Among the limitations of the study are the limited number of experts to agree on the recommendations of FARMAGER tool and the absence of other professionals involved in the preparation of the table. Also the unicentric nature of the study is another limitation. However, the extensive experience of our hospital pharmacy service in the reconciliation, treatment review and knowledge of optimization strategies and the establishment of a multidisciplinary team which allows to provide a global and targeted approach to the revision of the treatments of elderly patients can be consider a strength of our study.
The project of this study was granted a development financing by the Spanish Society of Hospital Pharmacy
The authors declare no conflict of interest
Bibliography
- Dequito AB, Mol PGM, van Doormaal JE, Zaal RJ, van den Bemt PMLA, Haaijer-Ruskamp FM, et al. Preventable and Non-Preventable Adverse Drug Events in Hospitalized Patients: A Prospective Chart Review in the Netherlands. Drug Safety. 2011 Nov;34(11):1089–100.
- Gellad WF, Grenard JL, Marcum ZA. A Systematic Review of Barriers to Medication Adherence in the Elderly: Looking Beyond Cost and Regimen Complexity. The American Journal of Geriatric Pharmacotherapy. 2011 Feb;9(1):11–23
- Vogeli C, Shields AE, Lee TA, Gibson TB, Marder WD, Weiss KB, et al. Multiple Chronic Conditions: Prevalence, Health Consequences, and Implications for Quality, Care Management, and Costs. J GEN INTERN MED. 2007 Dec;22(S3):391–5.
- Unutmaz G, Soysal P, Tuven B, Isik AT. Costs of medication in older patients: before and after comprehensive geriatric assessment. CIA. 2018 Apr;Volume 13:607–13.
- Gutiérrez‐Valencia M, Izquierdo M, Beobide‐Telleria I, Ferro‐Uriguen A, Alonso‐Renedo J, Casas‐Herrero Á, et al. Medicine optimization strategy in an acute geriatric unit: The pharmacist in the geriatric team. Geriatr Gerontol Int. 2019 Jun;19(6):530–6.
- Hanlon JT, Schmader KE, Semla TP. Update of Studies on Drug-Related Problems in Older Adults. J Am Geriatr Soc. 2013 Aug;61(8):1365–8.
- Van der Linden L, Hias J, Dreessen L, Milisen K, Flamaing J, Spriet I, et al. Medication review versus usual care to improve drug therapies in older inpatients not admitted to geriatric wards: a quasi-experimental study (RASP-IGCT). BMC Geriatr. 2018 Dec;18(1):155.
- Hilmer SN, Gnjidic D, Abernethy DR. Pharmacoepidemiology in the Postmarketing Assessment of the Safety and Efficacy of Drugs in Older Adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2012 Feb 1;67A(2):181–8.
- Palmer K, Villani ER, Vetrano DL, Cherubini A, Cruz-Jentoft AJ, Curtin D, et al. Association of polypharmacy and hyperpolypharmacy with frailty states: a systematic review and meta-analysis. Eur Geriatr Med. 2019 Feb;10(1):9–36.
- Patterson SM, Hughes C, Kerse N, Cardwell CR, Bradley MC. Interventions to improve the appropriate use of polypharmacy for older people. In: The Cochrane Collaboration, editor. Cochrane Database of Systematic Reviews [Internet]. Chichester, UK: John Wiley & Sons, Ltd; 2012 [cited 2021 Apr 27]. p. CD008165.pub2. Available from: http://doi.wiley.com/10.1002/14651858.CD008165.pub2
- By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults: 2019 AGS BEERS CRITERIA® UPDATE EXPERT PANEL. J Am Geriatr Soc. 2019 Apr;67(4):674–94.
- Delgado-Silveira E, Mateos-Nozal J, Muñoz García M, Rexach Cano L, Vélez-Díaz-Pallarés M, Albeniz López J, et al. [Inappropriate drug use in palliative care: SPANISH version of the STOPP-Frail criteria (STOPP-Pal)]. Revista Española de Geriatría y Gerontología. 2019 May;54(3):151–5.
- Rodríguez-Pérez, Aitana, Eva Rocío Alfaro-Lara, Sandra Albiñana-Perez, María Dolores Nieto-Martín, Jesús Díez-Manglano, Concepción Pérez-Guerrero, and Bernardo Santos-Ramos. ‘Novel Tool for Deprescribing in Chronic Patients with Multimorbidity: List of Evidence-Based Deprescribing for Chronic Patients Criteria: LESS-CHRON Criteria’. Geriatrics & Gerontology International 17, no. 11 (November 2017): 2200–2207. https://doi.org/10.1111/ggi.13062.
- [Pharmacogeriatric Guide of the Autonomic Community of Madrid] Ref 20224. Madrid: Servicio madrileño de Salud. Consejería Nacional de la Agencia Madrileña de Atención Social. Consejería de políticas sociales y familia. [Internet] [Cited 28 Apr 2021]; [about 550 p.]. Available from https://www.comunidad.madrid/publicacion/ref/20224
- [Spironolactone and Risk of Hyperkalemia]. Ref MUH (FV), 22/2011 [Internet] AEMPS. 2011 Nov 4th [Cited 28 Apr 2021]; [about 2 p.]. Available from https://www.aemps.gob.es/informa/notasinformativas/medicamentosusohumano-3/seguridad-1/2011/ni-muh_22-2011/
- [Zolpidem (Dalparan®, Stilnox®, Zolpidem EFG®): risk of somnolence the following day]. Ref MUH (FV), 5/2014 [Internet] AEMPS. 2014 Mar 11th [Cited 28 Apr 2021]; [about 2 p.]. Available from https://www.aemps.gob.es/informa/notasinformativas/medicamentosusohumano-3/seguridad-1/2014/ni-muh_fv_05-2014-zolpidem/
- [Citalopram and electrocardiogram QT interval prolongation] Ref MUH (FV), 19/2011. [Internet] AEMPS. 2011 Oct 27th. [Cited 28 Apr 2021]; [about 2 p.]. Available from https://www.aemps.gob.es/informa/notasinformativas/medicamentosusohumano-3/seguridad-1/2011/ni-muh_19-2011-2/
- [Escitalopram: prolongation of the electrocardiogram QT interval] Ref MUH (FV), 23/2011 [Internet] AEMPS 2011 Dec 2nd. [Cited 28 Apr 2021]; [about 2 p.]. Available from: https://www.aemps.gob.es/informa/notasinformativas/medicamentosusohumano-3/seguridad-1/2011/ni-muh_23-201
- [Domperidone and cardiac risk] Ref MUH (FV), 24/2011 [Internet] AEMPS. 2011 Dec 14th. [Cited 28 Apr 2021]; [about 2 p.]. Available from: https://www.aemps.gob.es/informa/notasinformativas/medicamentosusohumano-3/seguridad-1/2011/ni-muh_24-2011/
- [Bisphosphonates and risk of atypical femur fractures] Ref MUH (FV) /04/2011 [Internet] AEMPS. 2011 Apr 15th. [Cited 28 Apr 2021]; [about 2 p.]. Available from: https://www.aemps.gob.es/informa/notasinformativas/medicamentosusohumano-3/seguridad-1/2011/ni-muh_04-2011/
- [Cardiovascular risk of high doses of ibuprofen or dexibuprofen: recommendations for use] Ref MUH (FV), 4/2015 [InternetAEMPS. 2015 Apr 13th. [Cited 28 Apr 2021]; [about 2 p.]. Available from: https://www.aemps.gob.es/informa/notasinformativas/medicamentosusohumano-3/seguridad-1/2015/ni-muh_fv_04-ibuprofeno-dexibuprofeno/
- Hedna K, Hakkarainen KM, Gyllensten H, Jönsson AK, Petzold M, Hägg S. Potentially inappropriate prescribing and adverse drug reactions in the elderly: a population-based study. Eur J Clin Pharmacol. 2015 Dec;71(12):1525–33.
- Kara Ö, Arık G, Kızılarslanoglu MC, Kılıc MK, Varan HD, Sümer F, et al. Potentially inappropriate prescribing according to the STOPP/START criteria for older adults. Aging Clin Exp Res. 2016 Aug;28(4):761–8.
- Marrin-Gorricho R, Casajus-navasal A, Carrillo-Acevedo L, Serrano-Pérez A, Barajas-Santos MT, Hurtado-Gómez MF. Análisis de la prescripción potencialmente inadecuada según los criterios STOPP/START en un centro sociosanitario. Pharm Care Esp 2017; 19(6): 499-520.
- Moriel MC, Pardo J, Catalá RM, Segura M. Estudio prospectivo de conciliación de medicación en pacientes de traumatología. Farm Hosp. 2008;32(2):65-70
- Martín-Pérez M, López de Andrés A, Hernández-Barrera V, Jiménez-García R, Jiménez-Trujillo I, Palacios-Ceña D, et al. Prevalencia de polifarmacia en la población mayor de 65 años en España: análisis de las encuestas nacionales de salud 2006 y 2011/12. Rev Esp Geriatric Gerontol 2017; 52(1): 2-8.
- Palagyi A, Keay L, Harper J, Potter J, Lindley RI. Barricades and brickwalls –a qualitative study exploring perceptions of medication use and deprescribing in long-term care. BMC Geriatric 2016; 15: 16: 15.
- Scott IA, Hilmer SN, Reeve E, Potler K, Le Couteur D, Rigby D, et al. Reducing inappropiate polypharmacy: the process of deprescribing. JAMA Intern Med 2015; 175(5): 827-34.
- Tommelein E, Mehuys E, Petrovic M Somers A, Colin P and Boussery K. Potentially inappropiate prescribing in community-dwelling older people across Europe: a systematic literatura review. Eur j Clin Pharmacol. 2015; 71: 1415-27
- Jokanovic N, Aslani P, Carter S, Duong M, Gnjidic D, Jansen J, et al. Development of consumer information leaflets for deprescribing in older hospital inpatients: a mixed-methods study. BMJ Open. 2019 Dec;9(12):e033303.