Panini AC, Teves MR, Garraza MH, Rapisarda AMP, Calderón CP
Farmacología. Facultad de Química, Bioquímica y Farmacia. Universidad Nacional de San Luis (Argentina)
____
Rev. OFIL 2016, 26;4:301-306
Fecha de recepción: 30/12/2015 – Fecha de aceptación: 25/08/2016
____
Correspondencia:
Alicia del Carmen Panini
Farmacología, Chacabuco y Pedernera
Universidad Nacional de San Luis
5700 San Luis (Argentina)
Correo electrónico: acpanini@unsl.edu.ar
____
SUMMARY
Objective: Perform a descriptive study that it to be useful for a periodic comparison of prescriptions and for characterization of consumption in a Mental Health School Hospital (MHSH) of Argentina, know the prescription profiles and thus promote and contribute to the rational use of medicines. The objectives were oriented to measure the magnitude of consumption of psychopharmacs and identify the drugs of first election.
Methodology: The study design included an observational, cross-sectional and retrospective analysis of prescriptions performed on patients who attended in period between 1 and July 31, 2014. The drugs were coded according to International ATC classification system and the diagnostics were coded according to the International Statistical Classification of Diseases and Related Health Problems (ICD-10).
Results: All medicines were indicated as mono-drugs. An altogether of 2060 medicines was prescribed in the 819 recipes, being 1,959 (95.10%) psychopharmacs. In 218 (26.62%) of these recipes one psychopharm was prescribed while. In the 586 (71.55%) remaining recipes, among 2 to 8. The average number of drugs per recipe was 2.44, higher than optimal value proposed by World Health Organization (≤2). The most frequently used drugs were Clonazepam, Olanzapine, Paroxetine, Magnesium valproate and Haloperidol. The 82.06% of main diagnoses were grouped in the category of Mental and behavioral disorders.
Conclusions: The results indicated that polypharmacy was elevated. Is necessary to deepen studies that involving the possible interactions between psychopharmacs used, the observation of possible causal relationships triggers of adverse reactions that lower the therapeutic adherence, the efficacy of treatment and causing a higher spending related to the public health.
Key Words: Mental Health School Hospital, Argentina, psychopharmacs prescription, rational use of medicines.
____
Introduction
A strategic plan for the management and establishment of a lasting and effective health policy has among its main objectives the rational use of resources, prioritizing the provision of better services with reduced cost. Medications are one of the resources, that in a matter of health policy, required of a rational use motivated by high employment, and thus provide the best treatment at a lower cost and with minimum risk; concluding in a better quality of life related to health1, therefore, the rational use of medicines has a significant importance for an effective health system2.
The impact of psychotropic drugs cost in the public health care represents a great economic burden. In recent years, your turnover in Argentina has increased rapidly. In 2015, the total turnover of Pharmaceutical Industry in Argentina Republic amounted $6,103 million pesos (approximately $407 million dollars)3-6.
The rational utilization of medicaments that acting on the central nervous system (CNS) has its principles in the knowledge of neurotransmission processes, because, predominantly, existing active principles act as regulators of synaptic transmission more that as regulators of nerve conduction7.
Studies of drug use belong to Pharmacoepidemiology or Epidemiology of drugs8 as objective to promote and facilitate rational use of medications9.
The aim of this study was to obtain an instrument that allows for periodic comparison of prescriptions and the characterization of consumption in a Mental Health School Hospital of Argentina (MHSH), know the prescription profiles and thus promote and contribute to the rational use of medicines. The objectives were oriented to measure the magnitude of consumption of psychopharmacs and identify the drugs of first election.
Methodology
The study design included an observational, cross-sectional and retrospective analysis of drug prescriptions performed on patients who attended in the MHSH, in the period between 1 and July 31, 2014.
In the MHSH are attended only ambulatory patients. Is an establishment economically dependent of national public administration and therefore without financial burden on the patient. This establishment is only for people who lack of private health coverage.
Clinical data were obtained by reviewing medical records from patients’ files that allowed for the assessment of the number of drugs prescribed per consultation day. In this study, all drugs were prescribed by generic name. The sample comprised those patients attending the medical services of MHSH.
The records were entered into a spreadsheet created in Microsoft Office Excel 2007 program (Microsoft, USA), which was used for analysis and determination of the absolute and relative frequencies of the variables.
The active pharmacologically components included in the prescriptions were coded according to International ATC classification system (Anatomical, Therapeutical and Chemical) that proposed by the World Health Organization9 and available in internet10. Therapeutic indications were coded according to the International Statistical Classification of Diseases and Related Health Problems (ICD-10) of the World Health Organization11. Professional prescribers were coded with the aim of anonymity.
Results
1. Demographic variable: sex
During the study period, 819 recipes were registered. The majority of patients were female (56.41%; n=462); while of the male sex were 41.88% (n=343); fourteen prescriptions lacked data concerning the sex of the patient (1.71%).
2. Prescription of medications
In 819 prescriptions, altogether 2,060 medicines were prescribed, of which 1,959 belonged to N group (95.10%). In the remaining 4.90%, several active ingredients that act on different organs or systems were included (A, B, C, J, M and R groups of the ATC classification).
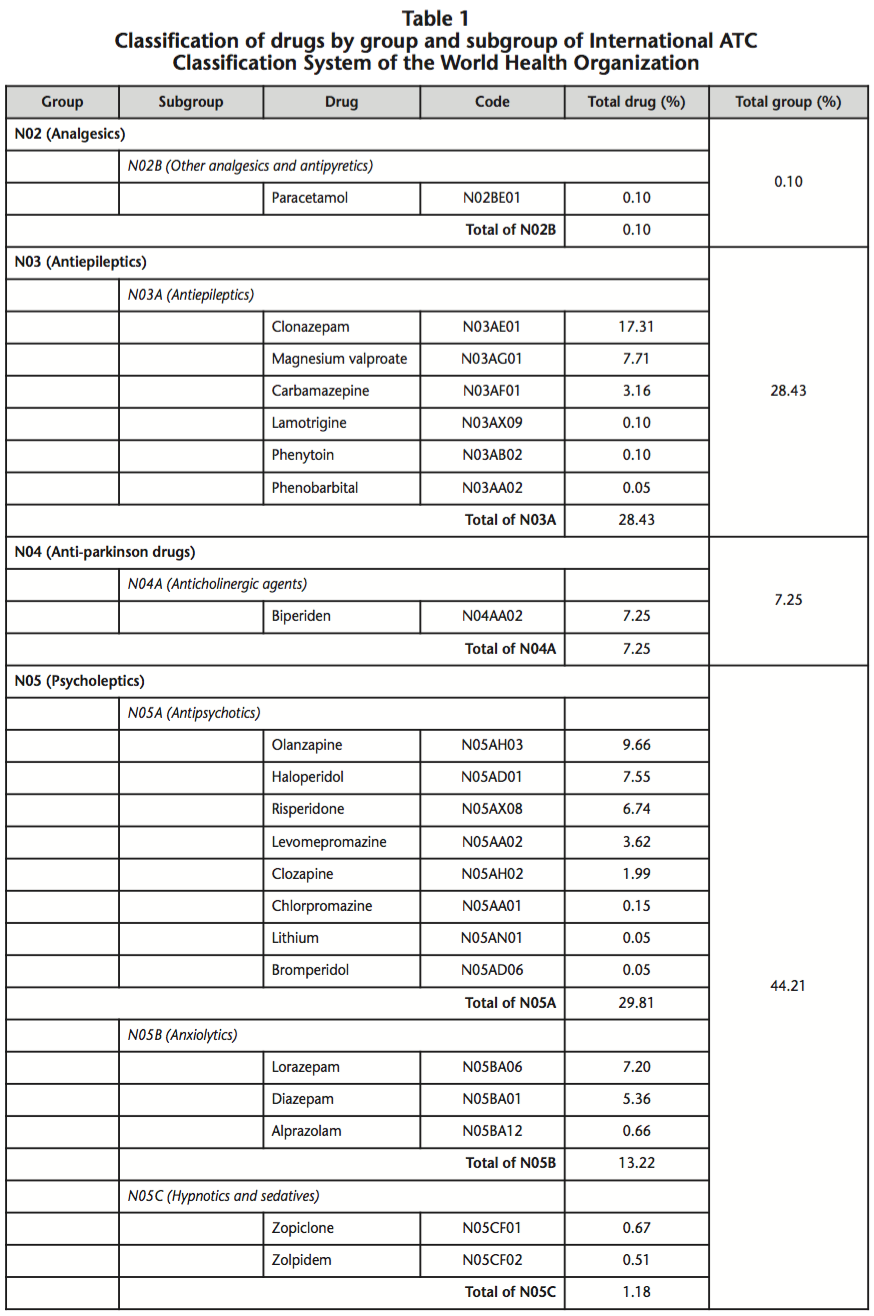
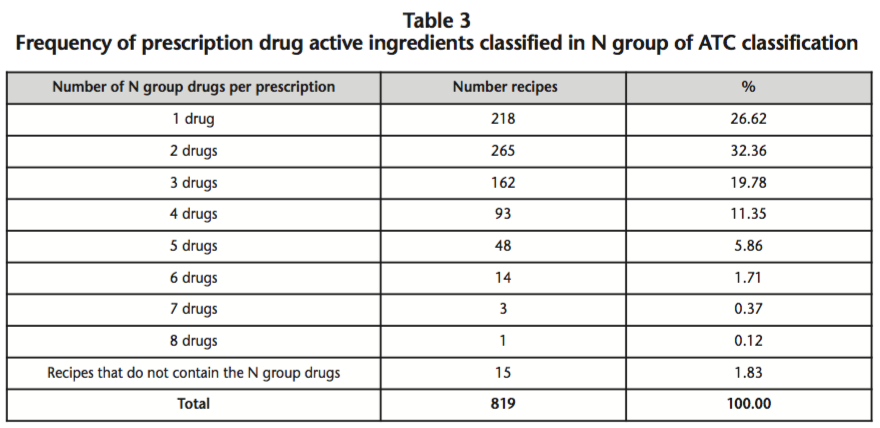
Of the analysis of recipes, is observed that 804 records (98.17%) have medicines that containing active substances whose mechanism of action involves interaction with pharmacological receptors located in the nervous system (N group) and only 15 recipes do not contain drugs of this group. Also within the group N, it is seen that subgroup N05 is who provides the greatest amount of prescribed drugs (44.21%) and in this subgroup, antipsychotics are the most commonly used. In table 1 are listed the psychopharmacs separated by group and subgroup of International ATC classification system, with the corresponding percentages.
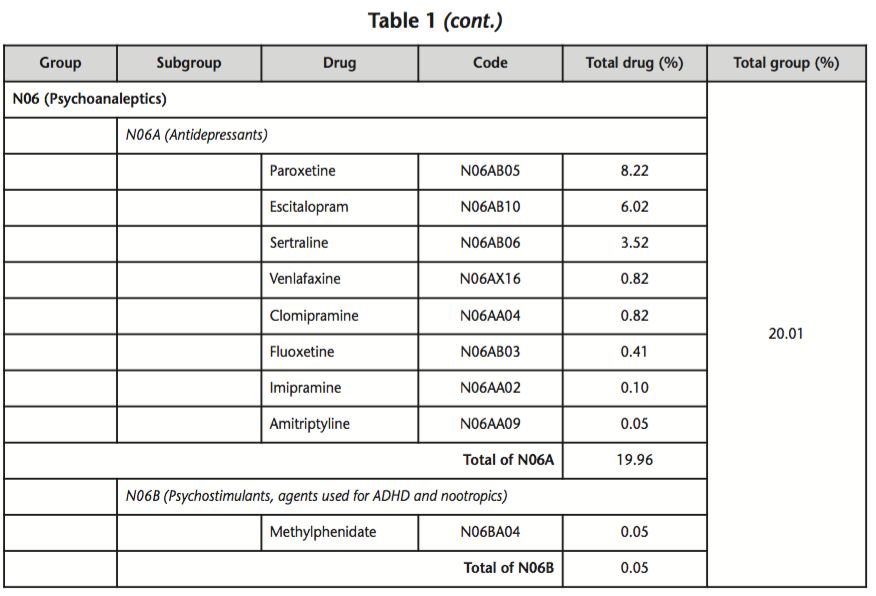
The most frequently used drugs were Clonazepam, followed by Olanzapine, Paroxetine, Magnesium valproate and Haloperidol, representing in together the 50.43% of the total active principles classified in N Group of ATC system. The percentages of prescription by these drugs, segregated according to the concentration, is showed in table 2.
3. Monotherapy versus Polypharmacy
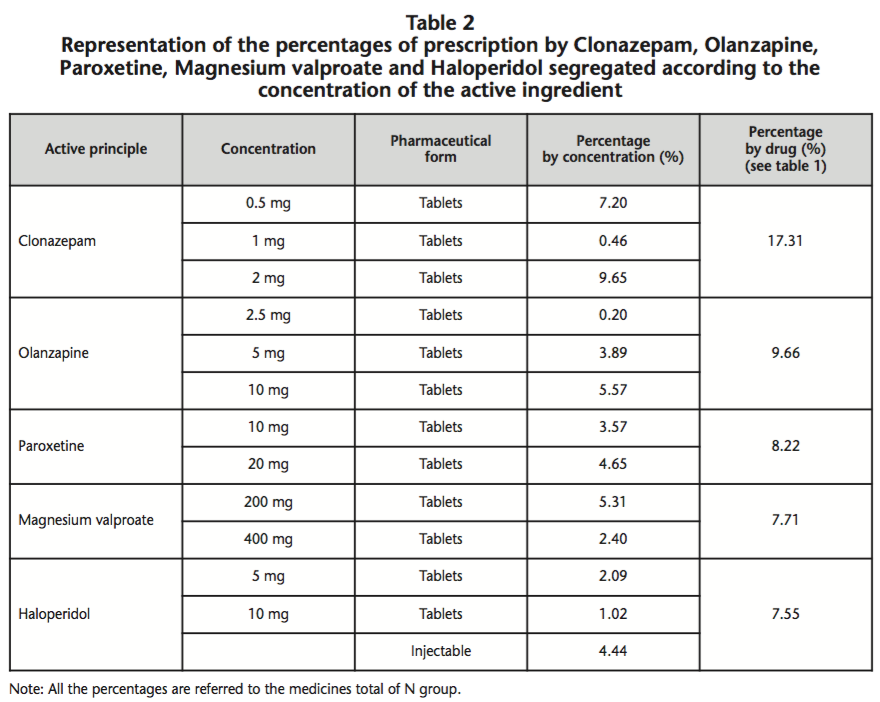
Only in 218 recipes (27.11%), one drug of group N was prescribed; in the remaining 586 (72.89%), to 2-8 drugs were prescribed (see table 3). The mean number of medications taken was 2.44 with a range of 1-8.
4. Therapeutic indications
The 82.06% (n=672) of main diagnoses associated with prescribed drugs were grouped in the category of Mental and behavioral disorders (F00-F99), 2.20% (n=18) with Diseases of the nervous system (G00-G99), 0.24% (n=2) Congenital malformations, deformations and chromosomal abnormalities (Q00-Q99) and 0.24% (n=2) with Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00-R99). In addition, a total of 125 recipes (15.26%) had no diagnosis or was not possible to decipher it (ND).
Of all diagnoses associated with the category of Mental and behavioral disorders, it found that anxiety (n=152; ICD-10: F41), psychotic disorders (n=122; ICD-10: F23), depression (n=88; ICD-10: F32) and adjustment disorders (n=55; ICD-10: 43) were therapeutic indications that motivated the highest number of drug prescriptions.
Discussion and Conclusions
Actually, the rational use of medicines is one of main objectives of health professionals. Is a strategy of World Health Organization and implies that patients receive medications appropriate to their clinical needs, in doses appropriates, during an adequate phase of time, and at the possible cost lowest12. The rational use of psychopharmacs imply getting the best effect with a reduced number of drugs, utilized during the shortest possible time and with at a reasonable cost, and for this purpose is essential assess the willingness of the patient to perform a good therapeutic adherence13.
Our results indicated that polypharmacy was elevated, being irrational or inadequate the use of too many medicines per patient12. In this study, the patients that were prescribed simultaneously with two or more psychopharmacs were considered as polymedicated. Despite the recommendations, the polypharmacy it is still widely extended around the world and in some cases, it is considered as a common practice, for example in the treatment of schizophrenia14. This is consistent with the information provided by Rittmannsberger15, who evaluated the use of drugs in the psychiatric inpatient, reporting a prevalence of 48% of monotherapy in investigations conducted before 1980, 31% between the years 1981-1990, and 20% between the years 1991-2000 in inpatients. Irrational use can be harmful for both the individual as to the population. A consequence of irrational use of drugs for public health and economy are the adverse effects that are able to produce, sometimes of lethal type, and generate an important morbidity and mortality. The costs estimated by hospitalization are elevated, generating a higher expenditure and consequently there is a loss of effectiveness in health policies. The medicines utilized to prevent adverse reactions of prescribed drugs in psychotic disorders, such as extrapyramidal side reactions are a reason that contribute to polypharmacy and its consequences.
In our analysis was found that only in 27.11% of recipes was prescribed monotherapy, which involves that of every four patients, three were object of polypharmacy.
In the present analysis of prescriptions the average number of drugs per recipe was 2.44, higher than optimal value of World Health Organization (≤2), similar result was founded in a study of rational use of medicines carried out in four government hospitals of United Arab Emirates16.
The adequate prescription of psychopharmacs is complex of to define, due that several factors influence in your prescription. The polypharmacy not always can be considered as an inadequate prescribing pattern, since the use more than one psychopharmacs can be effective in some individuals17.
The analysis of prescription records in MHSH, it indicates a high prevalence of diseases coded in the category of Mental and behavioral disorders, being anxiety, psychotic disorders, depression and adjustment disorders who motivated the highest number of drug prescriptions.
In general terms, there was a high predilection for Clonazepam, followed of Olanzapine, Paroxetine, Magnesium valproate and Haloperidol.
In antipsychotics group were preferentially prescribed atypical antipsychotics and those drugs whose mechanism of action is based on the antagonism of 5-HT2/D2 receptors (Olanzapine, Risperidone and Clozapine). Within antiepileptic drugs were mostly of election those who exercise their action on the GABA system (Magnesium valproate, Clonazepam and Phenobarbital) followed of those who exercise their action on sodium channels, stabilizing the membrane (Carbamazepine, Lamotrigine and Phenytoin). In antidepressants drugs were priority prescribed the Selective serotonin reuptake inhibitors (Paroxetine, Escitalopram, Sertraline and Fluoxetine)7.
Other authors also found that the use of more than one psychotropic drug seemed to be common, such as anxiolytics/hypnotics/sedatives and an antipsychotic drug prescribed simultaneously and antidepressants and an antipsychotic drug prescribed simultaneously18.
The principal limitation of our study was that a 15.26% of recipes had no diagnosis or was not possible to decipher it, and that this research involves alone those patients attending in MHSH, and therefore these results cannot be representative of national data. Furthermore, this was an observational, cross-sectional and retrospective, considering only the month of July, 2014 for the analysis of prescriptions. Although the sample analyzed may be considered small, were included all patients who attended the medical services of hospital.
We consider it necessary to deepen in studies involving the possible interactions between psychopharmacs used and furthermore in the observation of possible causal relationships triggers of adverse reactions that lower the therapeutic adherence, the efficacy of treatment and that cause a higher spending related to the public health.
Finally, worryingly the antipsychotic drugs are widely used for the treatment of different behavioral and psychological symptoms, despite their limited efficacy and safety.
Acknowledgments: This work has been supported by the following grant: research project: PROICO 2-0412, of the Secretaría de Ciencia y Tecnología of Universidad Nacional de San Luis, Argentina.
Competing interests: The authors declare no conflicts of interest.
Bibliography
1. Provencio RM. Estudios de utilización de medicamentos. Revista de Neurología (Barcelona) 1996;24 (128):397-9.
2. Khan M, Ara N. Promoting rational prescribing among medical practitioners. Bangladesh Medical Journal 2014;40(2):6-7.
3. National Institute of Statistics and Census of Argentina Republic. First quarter report 2015 [internet]. Buenos Aires; 09/06/2015[cited July 28, 2016]. Available at URL: http://www.indec.gov.ar/uploads/informesdeprensa/farm_06_15.pdf.
4. National Institute of Statistics and Census of Argentina Republic. Second quarter report 2015 [internet]. Buenos Aires; 08/09/2015 [cited July 28, 2016]. Available at URL: http://www.indec.gov.ar/uploads/informesdeprensa/farm_09_15.pdf.
5. National Institute of Statistics and Census of Argentina Republic. Third quarter report 2015 [internet]. Buenos Aires; 02/12/2015 [cited July 28, 2016]. Available at URL: http://www.indec.gov.ar/uploads/informesdeprensa/farm_12_15.pdf.
6. National Institute of Statistics and Census of Argentina Republic. Fourth quarter report 2015 [internet]. Buenos Aires; 10/05/2016 [cited July 28, 2016]. Available at URL: http://www.indec.gov.ar/uploads/informesdeprensa/farm_05_16.pdf.
7. Lorenzo P, Moreno A, Lizasoain I, Leza JC, Moro MA, Portolés A. Farmacología básica y clínica/Velázquez. 18.a ed. Madrid: Médica Panamericana; 2008.
8. Martín Arias LH. Estudios de utilización de medicamentos. En: Carvajal García-Pando, A. (Coord.). Farmacoepidemiología. España: Secretariado de Publicaciones, Universidad de Valladolid; 1993.
9. World Health Organization. Introduction to Drug Utilization Research. Oslo, Norway; 2003.
10. World Health Organization, Collaborating Centre for Drug Statistics Methodology [internet]. Guidelines for ATC classification and DDD assignment, 2015. ATC/DDD Index 2015 [cited August 22, 2015]. Available at URL: http://www.whocc.no/atc_ddd_index/.
11. Pan American Health Organization. Clasificación estadística internacional de enfermedades y problemas relacionados con la salud. 10a. revisión, 3 vol. Washington D.C: Publicación Científica 554; 1995.
12. World Health Organization, Policy Perspectives on Medicine. Promoting rational use of medicines: core components [Internet]. Geneva; 2002. Available at URL: http://apps.who.int/medicinedocs/pdf/h3011e/h3011e.pdf.
13. Panini AC, Garraza MH, Teves MR, Giraudo E, Calderón CP. Use of Psychotropic Drugs: Between the Medicalization and Rationality. In: Gargiulo PA, Mesones-Arroyo HL, editors. Psychiatry and Neuroscience Update. Switzerland: Springer; 2015. p. 207-215.
14. Correll CU, Gallego JA. Antipsychotic polypharmacy: a comprehensive evaluation of relevant correlates of a long-standing clinical practice. Psychiatric Clinics of North America 2012;35(3):661-681.
15. Rittmannsberger H. The use of drug monotherapy in psychiatric inpatient treatment. Progress in Neuro-Psychopharmacology & Biological Psychiatry 2002; 26:547-551.
16. Mahmood A, Elnour AA, Ali AAA, Hassan NAGM, Shehab A, Bhagavathula AS. Evaluation of rational use of medicines (RUM) in four government hospitals in UAE. Saudi Pharmaceutical Journal 2016;24(2):189-196.
17. Kukreja S, Kalra G, Shah N, Shrivastava A. Polypharmacy in psychiatry: a review. Mens Sana Monographs 2013;11(1):82-99.
18. Gustafsson M, Karlsson S, Lövheim H. Inappropriate long-term use of antipsychotic drugs is common among people with dementia living in specialized care units. BMC Pharmacol Toxicol. 2013;14:10.
____
Download PDF: Prescription analysis on ambulatory patients in a Mental Health School Hospital of Argentina
